
In response to fertility problems among men and women, biomedical techniques associated with artificial insemination, in vitro fertilization and clinical therapy using application of drugs have been implemented under the broad category of Assisted Reproduction (ART). ART is a high technology procedure performed between the male sperms and female eggs through 3 commonly used techniques namely, In vitro fertilization (IVF), Gamete Intrafallopian Transfer (GIFT) and Zygote Intrafallopian Transfer (ZIFT). The scope of this discussion is, however, centered around the IVF therapy.
IVF encompasses all the techniques involving the retrieval of the sperm and egg from the male and female respectively, fertilizing them in artificially induced bodily conditions, culturing them in the laboratory to produce the zygote and introduce the zygote or the blastocyst back to the woman’s body. IVF also regulates the ovulation cycle of the woman undergoing the therapy to monitor the timing of ovulation and proceed with the steps that follow till the transfer of the embryos. IVF was first implemented in 1978 at England seeing the birth of the first test-tube ever and has evolved since then with the input of more advanced and developed technology in performing the procedure.
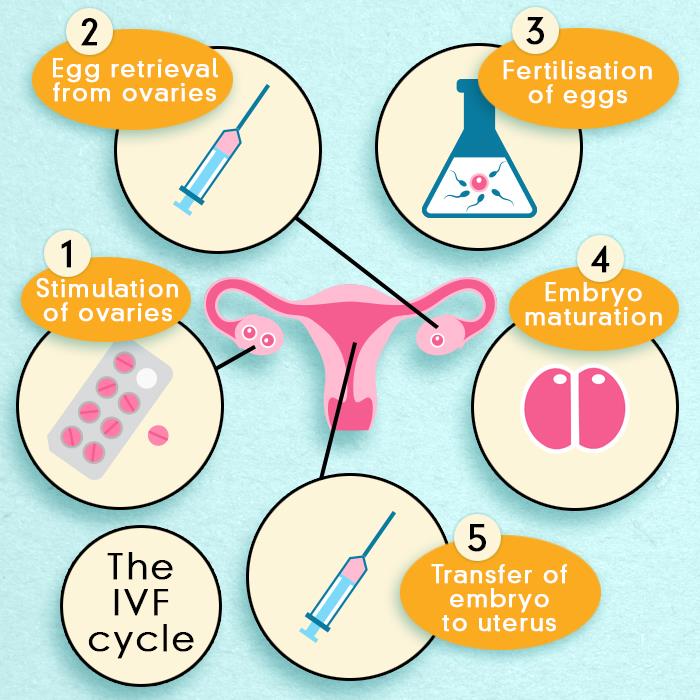
The multi-stage procedure of IVF therapy takes place following a sequence of successive events. These stepwise events have been discussed below
• Ovary stimulation and regulation of the ovarian cycle:
Hormonal supplements are given to the woman undergoing IVF to induce the development of a batch of follicles at a predetermined time window. Unlike the natural way, in which a single egg is produced every month, in these females, the stimulation triggers the development of multiple follicles and therefore, multiple eggs at the desired time. The importance of induction of ovulation lies in establishing a control over the timing of ovulation in the patient through the application of hormonal analogs. The dosage of these supplements and medications is regulated on the basis of the response of the body of the treatment. Thereby, when a certain stage of follicle generation is complete, all the medications are terminated and a specific hormone to trigger ovulation ie, the release of the egg from the ovary is initiated.
• Retrieval of egg:
Egg collection is performed either surgically from the ovary through the vagina or through ultrasound-guided aspiration. Local anesthetics are given to avoid causing any discomfort to the patient as the aspiration of the egg through a fine needle under ultrasound control is mediated. This procedure enables as many as 20 eggs to be harvested at a time. These eggs could be cultured for the subsequent steps of IVF or preserved in liquid nitrogen at low temperatures for future use.
• Fertilization:
After retrieval of the sperm and egg from the couple, they are cultured in the laboratory at a temperature same as that of the woman’s body. The collected semen is sampled and added to the ova in the culture dish. More commonly, Intra-cytoplasmic sperm injection (ICSI) is performed to isolate the sperm cell with a fine needle and inject it into the egg using a microscope. IVF accompanied by ICSI, facilitates micromanipulation thereby, enhancing the efficiency of the technique. Following approximately 40 hours of incubation, the eggs are observed to examine if they will have undergone fertilization and cell division. After careful examination, the healthy embryos are introduced into the woman’s uterus or frozen for future use. Generally, the defective embryos are discarded and the embryos which develop up to the eight-cell stage introduced into the woman’s uterus.
• Embryo transfer:
The final step in IVF is the transfer of the embryo into the uterus 2-3 days following the egg retrieval. Having divided till the 2 or 4 cell stage embryo, about 2 or 3 of these fertilized eggs are introduced into the uterus using ultrasound regulation, to maximize the success of pregnancy. When many embryos begin to grow simultaneously, the ones in excess are terminated.
A DIAGRAMMATIC REPRESENTATION OF THE IVF PROCEDURE
Having known the procedure of IVF, it becomes necessary now to understand and validate how this procedure could be of help to women and why it is worth all the money, medications, and hormones to be introduced to her body.
Firstly, it kindles a hope among couples with infertility problems, to bear a child of the same genetic identity as them, and therefore, their own. Women with blocked or damaged or missing fallopian tubes can resort to this method to have a baby of her own. Similarly, for men with low sperm count, abnormal sperm structure, motility or spinal cord injury, this procedure could be a boon in disguise. Next, the embryos produced by this technique show normal development and are appropriate for implantation. Resistant to possible teratogenic insult, malformations or abnormal development of embryos during IVF is a rarity. Genetic screening of the embryos prior to implantation further can help detect genetic anomalies in the embryo produced.
The donation of eggs and egg collection is a pre-requisite for performing IVF. However, these eggs once collected could be preserved for future use without having to perform the retrieval all over again. In fact, this is an additional advantage for mothers undergoing chemotherapy to preserve their eggs for the future. Also, in certain cases, IVF can be combined with surrogacy to facilitate the birth of a baby. Similarly, sperm or semen collection can also be implemented by the biological father or a donor as per the requirement of the situation. Lastly, IVF has great prospects in contributing to the advancement of stem cell research using the embryos which are not used for implantation.
However, in spite of all the known advantages of performing IVF, the biggest disadvantage of the procedure is its low rate of success which is only about 20% in spite of the exorbitant expenditure underlying the entire procedure. To maximize the success of the procedure even though 2 to 3 of the embryos may be implanted, this strategy may, in turn, lead to multiple births. Multiple pregnancies can be a matter of great concern for both the mother and baby. The lack of technology to initiate embryo implantation directly into the uterus has further led to the uncertainty regarding successful implantation which is a matter of chance. The increased risk of ectopic pregnancy due to implantation in the abdominal cavity or fallopian tube can thus result.
With the increased exposure of the mother to the side effects of hormone analogs and drugs poses risk to her health. Most commonly, the ovarian hyperstimulation syndrome impacts the mother’s health due to the accumulation of body fluids in the abdominal cavity interfering with the normal functioning of the respiratory and circulatory system. Also, IVF-conceived children may be at a greater risk of developing cardiovascular and skeletomuscular defects.
Besides, the ethical concerns governing the IVF procedure are many. Not only are these issues considered by some to be unnatural and hence inhuman, since it is an attempt to create life artificially in the laboratory by exposure to foreign chemicals. Also, the discarding of defective embryos and making a selection of the healthy embryos for implantation is considered to be unfair and immoral on the basis of its equivalence to abortion.
Therefore, knowing the exact benefits and disadvantages of IVF, most of the women are caught in an inner conflict to have to make a choice between being gifted by a baby or to fight her way through many possible risks to have a baby through IVF.
